Institute of Pathology/National Museum of Health and Medicine, distributed via the Associated
Press, Public domain, via Wikimedia Commons
As the COVID-19 pandemic stretches into 2021, people are looking for lessons from the past to understand the present. The so-called “Spanish flu” of 1918 provides an important point of reference. The 1918 pandemic was one of the deadliest in human history with upwards of 50 million people dying from influenza. Moreover, it was estimated that as much as a third of the world’s population was infected. While Canada was hit less severely, it is estimated that 50,000 people died from influenza, with the real numbers certainly being higher due to the spotty reporting of cases at the time. The great majority of these deaths occurred during the global second wave from September to December 1918—an important fact to note as we pass through the second wave of COVID-19. Regardless of comparisons to other countries, it is hard to take this death toll as a modest sum. In just a few months, almost as many Canadians died from influenza as in all five years of the First World War. In communities like Okak and Hebron in Labrador, the virus left a more traumatic legacy than the war ever could.
The invoking of the 1918 pandemic in 2020-21 also invites many questions. The 1918 pandemic was not humanity’s first encounter with a global plague and not even the first influenza pandemic, but much has changed in the intervening century. There have been many advances in medical research and virology. Moreover, we are capable of producing more than ever before as a society. Why, then, were so many countries caught so off-guard, under-resourced, and unprepared that some experts were projecting as many as 30 to 70 per cent of national populations might become infected? It is this question that really makes it worthwhile to look at the history of the 1918 pandemic and see the comparisons that exist with it today.
Pandemics are not historical accidents and the ones that began in 1918 and 2020 are no exceptions. The influenza virus of 1918 was not created by humans, but by an imperialist war, poor living conditions for the working class across the globe, and a lack of will to fight the pandemic, which greatly amplified both the spread and lethality of the virus. These three factors were all products of the system the pandemic occurred within, that of capitalism. And while capitalism did not create the virus, it can be said to have created the epidemic, both in 1918 and in 2020.
What do we know about the ‘Spanish flu’?
Before delving deeper into the 1918 pandemic, it is worthwhile examining what exactly the Spanish flu was. For one thing, the name itself is a misnomer. There is no evidence the virus originated in Spain. It appears to be no more than a racist pejorative that arose from large infection numbers and some high-profile cases coming from Spain. The only purpose the name seemed to serve was to try to lay blame for the virus on an ethnic group, in a manner not dissimilar from the way those using the term “Chinese virus” for the novel coronavirus do today.
In terms of the actual origins of the influenza virus, it is thought to have come from a pig and is seen as quite similar to the “swine flu” virus of 2009. Many of the symptoms of the virus itself were not that different from other flu viruses. If there was one thing peculiar about this strain of the flu, it was that unlike other viruses that prove most lethal to the elderly, it was most deadly to people of working age. For instance, in Saskatchewan, people between the ages of 20 and 40 comprised 57.8 per cent percent of deaths. Historians attribute part of the reason for this to a previous influenza epidemic in 1890, which conveyed some resistance to those alive at that time.
How an imperialist war spread influenza across the world

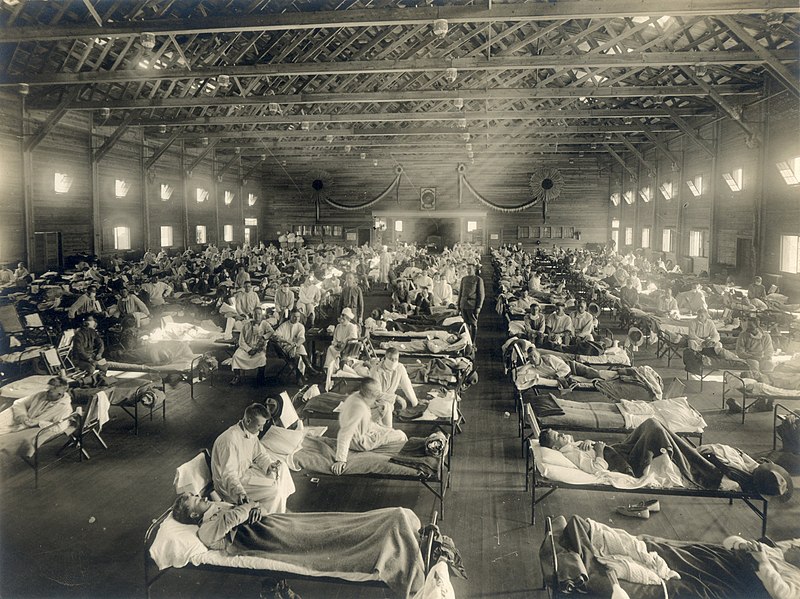
camp during World War I. Source: Nurse Gertrude Smith, Public
domain, via Wikimedia Commons
For a long time there has been a soft consensus that the first human cases of the virus originated in rural Kansas in January 1918, with spread ramping up when the first outbreak developed in a military base in the state in March 1918. Due to failures to properly contain this initial outbreak, it is thought to have served as the basis for eventual spread to the rest of the United States and Europe. The large movement of troops and war material back and forth from the U.S. to Europe as part of the American Expeditionary Force joining the war effort in Europe has been blamed for causing the rapid spread of the virus. Trench systems, army encampments, and military hospitals in Europe served as centres for new outbreaks. The imperialist war was therefore responsible for significantly exacerbating the pandemic.
Some studies suggest alternative origins for the first outbreak. One alternative points to an unidentified virus that spread across rural regions in the interior of China in 1916 and 1917. A second alternative looks to a virus with flu-like symptoms in the Pas-de-Calais department of France in 1916 as the originating point. However, neither alternate point of origin changes the centrality of World War I in spreading the virus. When it comes to the former, historians have suggested it was the Chinese Labour Corps being sent to support the war effort on the Western Front that fueled the early global dispersion. The latter hypothesis suggests that the first outbreak in the Pas-de-Calais was in a British Expeditionary Force field hospital, with subsequent outbreaks in other military facilities furthering spread until it became a pandemic. Taken in totality, regardless of which point of origin is taken, there is little doubt an imperialist war played an important role in the early spread of one of the deadliest pandemics in human history.
How the war effort spread the virus across Canada
World War I would also play an important role when it came to both the arrival of the initial influenza cases to Canada and in the subsequent spread across the country. While Newfoundland, not yet a part of Canada, was hit by the first global wave of the virus, there is little definitive evidence that there was any substantive spread of influenza in Canada proper at the time. However, Canada would not escape the second wave, with the first outbreaks developing in September 1918.
Research by Mark Humphries, a Canadian historian of the war and the pandemic, has identified four initial locations where influenza first arrived in Canada. These sites were in Niagara-on-the-Lake in Ontario, Saint-Jean and Victoriaville in Quebec, and Sydney, Nova Scotia. Perhaps the most pertinent fact about the initial outbreaks at these sites is that at least three of them were tied to the movement and training of American troops on the way to the Western Front.
The war effort played an even more important role in the rapid diffusion of the virus across Canada. As Humphries’ research concludes, the primary catalyst for spread within Canada appears to be the transport of the Siberian Expeditionary Force (SEF) by train across the country in its failed mission to help the White armies overthrow the Russian Revolution. The first cases are thought to have been brought on board in Sussex, New Brunswick, with sick soldiers exiting the train across the country starting in Montreal. It is this train that is thought to have brought the first cases to the barracks in Winnipeg on Sept. 28, followed by more initial cases to Regina, Calgary, and Vancouver. It did not help that the movement of the SEF was kept secret, meaning many of these towns were unaware that a train was arriving from areas where the virus was spreading in Eastern Canada. It is for this reason that Humphries quite correctly asserts that Canada’s increasing commitment to the war in Europe was to blame for the rapid spread of influenza in 1918. It is one of many ways that capitalism is at fault for the spread and severity of the epidemic.
How the virus impacted Canada

Source: Unknown author, Public domain, via Wikimedia Commons
As with many other features of the two pandemics, there are some similarities to the way influenza hit Canada in 1918 and how the novel coronavirus did in 2020. For instance, P.E.I. responded similarly in 1918 by shutting off access to the island and thereby limited spread of the virus. On the other end of the results spectrum in terms of total cases and deaths, Quebec was the worst hit province in 1918. A particularly bad outbreak occurred in Montreal due to an inept response that resulted in at least 17,000 cases and more than 3,000 recorded deaths in the city. The new Prairie provinces of Alberta and Saskatchewan, under-resourced with a dispersed and rapidly growing population, saw mortality rates nearly twice the national average. In what is a tragically common theme throughout Canadian history, some Indigenous communities were among the worst impacted due to the privations created by colonialism, amplified by a government leaving them to handle the epidemic alone. Consequently, the virus ravaged several Indigenous communities across the country from Okak, Labrador, where 150 people in a population of 220 died, to Christian Island in Georgian Bay, where 48 out of a population of 275 died. The trauma and death these communities endured is just one more injury in a long list of injustices that Indigenous people have faced in Canada.
For everyone living through the current pandemic, it is of little comfort that there appear to be many similarities to the response in 1918 and 2020. For instance, in an example that was repeated in other cities across the country, Edmonton required that masks be worn in public from Oct. 25 to Nov. 23, 1918. However, this requirement was not implemented everywhere, with some provinces such as New Brunswick making masks optional. Some health officials, such as Toronto Medical Officer of Health Charles Hastings, opposed masks despite growing evidence that they were effective in limiting spread.
Varied attempts were also made to reduce spread by requiring the quarantining of cases and containment of outbreaks. This was coupled with regulations to limit movement between cities and provinces. These two measures, when taken together and in a timely manner, proved to be an effective response. One good example is P.E.I., which closed off access to the province in October 1918 as cases began to appear in Atlantic Canada—a response that echoes the one in 2020. As a result of this early action, the province was successful in containing the virus with no observable increase in mortality during the epidemic. Finally, there were mixed efforts to shut down stores, factories and churches, and to limit public gatherings. However, like today, this patchwork of measures often came too late and was watered down by the interests of business owners and demands to support the war effort.
Vaccination proved to be one of the most effective responses to the virus in places where a vaccine was quickly developed. In Manitoba, two separate “live” vaccines were developed simultaneously by the province and military officials in October 1918 using diluted cultures of the virus. Those vaccinated experienced much less severe symptoms and a lower mortality rate if they did eventually become infected by influenza. Unfortunately, vaccines were not distributed across the country and in some areas produced vaccines were left unused due to poor uptake from lack of outreach. It seems as if today’s capitalists are incapable of learning from this history.
The failure to respond: Profits and war came first, fighting the virus second
While going through all the measures put in place to respond to the influenza epidemic can leave a flattering picture, the reality of the response left much to be desired. Undoubtedly part of this can be attributed to the medical field struggling to come to terms with how to effectively combat viruses. However, even accounting for this uncertainty, many approaches that were known to work were not implemented or were put in place too late. Furthermore, there was little direction or central coordination to the response and insufficient resources were directed to fighting the virus. One thing that is clear about the response is that the interests of the bosses and supporting their imperialist war in Europe was the priority. Fighting the spread of the virus was of secondary importance.
One good example of this failure to respond is seen in how a centuries-old method of fighting infectious diseases was used: that of quarantining, isolating, and placarding cases. While quarantining outbreaks and isolating individual cases was increasingly acknowledged to be a good method of limiting the spread of the virus in the U.S., this could only be effective if it was done early and properly supported. Alas, many city officials and public health officers in Canada threw their hands in the air and said this was impractical, that they did not have the resources to do so. To them the virus was a force of nature that would sweep through their cities regardless of action. Others waited too long to implement quarantine measures and then decried them as futile when they inevitably failed. This recklessness was so extreme in some cases, such as in Vancouver, that other cities like Victoria were actively appealing to the province to quarantine the city from the rest of the province.
It is also worth mentioning that the atrocious conditions that the capitalist class forced on the working class played a part in the reluctance to isolate influenza cases. Some doctors actively resisted requirements to report and isolate cases for fear that many workers would not seek medical help if this was required. Why would workers resist medical help and isolation? It is quite simple. There was no Employment Insurance or any other support for those unable to work in Canada in 1918, other than charity. For many workers that became ill, isolation could mean starvation for themselves and their families.
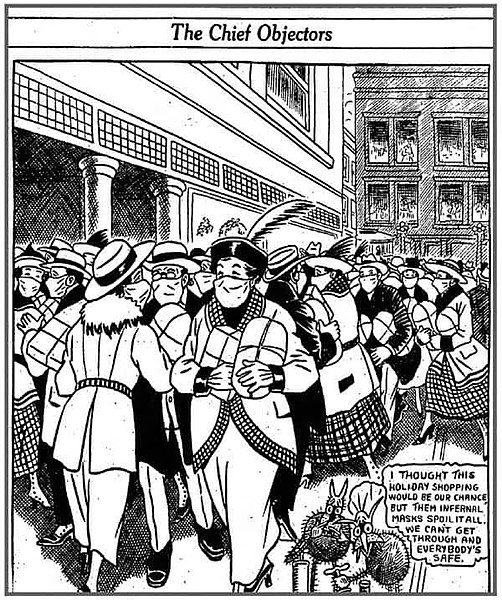
signature nor attribution seen., Public domain, via Wikimedia
Commons
Moreover, isolating infected people and limiting spread within housing that was cramped and lacked proper sanitation facilities was completely impractical. It is little surprise that Montreal was an epicentre for the spread of influenza if one considers the conditions that the working class lived in. One historian related the health risks inherent in the housing situation at the turn of the century:
Overcrowding and house or apartment sharing were another feature of the Montreal housing market that doctors and sanitary officials identified as the leading cause of the spread of illness and of child and adult deaths.
In other cities, similar conditions also resulted in more deaths. The northern part of Winnipeg, an area of the city with a large working-class immigrant population, was primed to be hit hard by a virus due to a lack of clean water, no proper sewage systems, and overcrowding. It was these conditions that saw it suffer from one of the highest mortality rates in the world during a typhoid epidemic from 1904 to 1905. It would fare little better in 1918, with a mortality rate of 6.73 per 1,000—more than 50 per cent higher than the 4.02 per 1,000 seen in the more affluent south of the city.
Another issue seen in 2020 that was also present in 1918 was the resistance in many cities and towns, often led by business owners, to the closure of factories, stores, schools, and churches. One particularly egregious example was that of Montreal. As new cases and deaths began to ramp up starting in late September into early October, the public health board of the city refused to order any significant closures until Oct. 7—and even then these were diluted by concessions to the lobbying of business owners. Only after a public outcry that saw health board members replaced on Oct. 10, so that the board was comprised solely of doctors, were any substantive measures taken. By then there were close to 1,000 reported cases in the city and at least 226 deaths, with the real numbers certainly being higher. The recorded case numbers would peak shortly afterwards on Oct. 15 with a single-day record of 1,868 cases. This lay bare the reality that the public health measures taken represented too little and came way too late.
The desire to keep making profits for capitalists during an epidemic was repeated across the country, with factories continuing to operate from Toronto to Winnipeg to Vancouver despite warnings that the close confines and poor ventilation in them were a recipe for spread. As a result, workplaces like the telephone exchange in Winnipeg, which saw 25 of 75 workers catch influenza, became centres for local outbreaks. Some bosses, such as those at the Canadian Pacific Railway (CPR), had plenty of blood on their hands. On Nov. 6, a report by the CPR stated that 2,270 workers on its western lines were sick. This alone is a shockingly high total for a virus that represented a real threat to people of working age. Furthermore, one cannot seriously examine the high mortality rates in Saskatchewan and Alberta without taking into the account the role that the CPR played in those provinces, and the large number of infections amongst their workers.
Whether to close schools was a subject of much debate too, and many of the same local officials that resisted closure of businesses were also reluctant to close schools. As influenza spread rapidly in the city and absenteeism in schools increased, Vancouver’s public health officer, Frederick Underhill, aligned with city bureaucrats and local business leaders to actively frustrate attempts to close schools. It is also pertinent to point out that public health officials fighting to keep schools open cited the welfare of children as their primary rationale. This too is something that is repeated today. From Underhill in Vancouver to Ontario Chief Medical Officer John McCullough, officials spoke ominously of the danger of children being left to “roam the streets” and the threat this represented to their development.
Passing the buck: How workers were left alone to fight the virus
One of the biggest failures in 1918 was the failure to act. In 1918 there was no Federal Department of Health, and one was not created until after World War I ended. Consequently, the federal government was largely missing in action in accounts of the epidemic and there is little evidence direction or extra resources were given to provinces and cities. This complete absence reflected a certain indifference amongst the ruling class in Canada to the many deaths the virus caused.
The response was little better at the provincial level. The only province to have a department of health at this time was New Brunswick and that one was newly christened, only coming into place at the start of the epidemic in October 1918. This left the responsibility to act to the various provincial public health boards. These boards made up a patchy framework of different regulations and powers across the country that were often not fit for the challenge they faced. One of the things the pandemic in 2020 has underlined is how important reporting and tracking a virus is to limit spread. However, in September 1918, as the first influenza cases were being identified in Ontario months into a global pandemic, influenza was still not required to be reported by health officials under the Ontario Public Health Act of 1912. Moreover, there seems to be little evidence of any coordination between provinces in their response to a virus that knew no borders. It is clear many of these boards were ill-prepared to act.

Source: Photographer not named, Public domain, via Wikimedia
Commons
The provincial boards often mimicked the callousness of the federal response by devolving the burden of action onto cities and towns, who were often poorly equipped. In New Brunswick, local health boards were required by the province to report cases and deaths. Unfortunately, reporting was scattershot due to the municipalities not having adequate medical workers to do this properly. Several community doctors overburdened with treating influenza patients were unable to do any reporting. In other municipalities, the burden fell on civil servants with no medical training who were unable to properly identify influenza cases. Despite this situation, there is no evidence that the provincial ministry of health stepped in to rectify the problem.
Some of the public health powers that were created never seem to have been properly employed. This reflected the lack of importance the health of workers meant for the ruling class and their bureaucrats. Keeping with the example of New Brunswick, legislation was passed in the province in 1898 and 1903 requiring some funding of public health units by municipalities. However, many municipalities did not follow through with these requirements and there was little pressure put upon them by the province to do so. In other instances, action came too late. In Saskatchewan the Union Hospital Act, a piece of legislation that allowed rural towns to pool resources to build hospitals, had just been passed in 1917. As a result, the population of Saskatchewan—which had expanded rapidly in the previous two decades and was almost entirely rural—was served by only eight hospitals in 1918. This made access to a hospital for sick people in the province very impractical. Saskatchewan’s lack of preparation and adequate health care facilities was reflected in other parts of Canada, with a few exceptions like Toronto.
The frequent reluctance of the bosses to make any significant sacrifices even came out at the local level. While cities across the country from Montreal to Vancouver set up makeshift hospitals and clinics with extra beds to treat influenza patients, their charity to the sick and unemployed often ended there. In several cities, relief efforts that saw meals delivered to the sick were led by unions, charities, and civil society groups, not the municipality. In Winnipeg, faced with a growing number of sick, furloughed, and unemployed workers, labour leaders appealed to the city council for help, noting the sacrifices these workers had made to fight the spread of the virus. A historian of the epidemic in Canada, Esyllt Jones, summarized their reply, noting that “callous city officials responded by saying everyone had to do their bit” while rejecting the demands made. These words foreshadow the rhetoric of politicians today, appealing to workers that “we are all in this together” while their timidity in action belies those very words. It was the working class that made sacrifices and put their health at risk to fight a pandemic, while the bourgeoisie put their interests first. This rejected appeal was not forgotten by workers in Winnipeg. Just a few months later, more and more workers began dropping their tools and going to the picket line as the Winnipeg General Strike picked up momentum in 1919.
Why capitalism caused the epidemic
Going through their response leaves little doubt there was a lack of will and substantive failings by the Canadian state to respond to the “Spanish flu” epidemic in 1918. Truthfully though, this failure was no historical accident. The spread and severity of the epidemic was enabled by a system defined by the dominant mode of production. That system was capitalism. It is a system built to serve the interests of a certain class, that of the bourgeoisie. Attempts to combat the virus were always subordinated to these interests. Furthermore, the social and material conditions that spawned from this mode of production only amplified the misery and death the virus caused. Fighting a global pandemic was not in the design.
One of the ways that capitalism quite literally enabled the spread of the virus has already been laid out namely, that the intensification of support for the imperialist war in Europe helped spread influenza across Canada. However, this is not the only reason the war effort was to blame. The lack of sanitation and poor conditions in the trenches in Europe created outbreaks amongst soldiers that served as a basis for further spread. Even once the virus was present in many towns and cities across Canada, other factors relating to World War I increased the spread and severity of the virus.
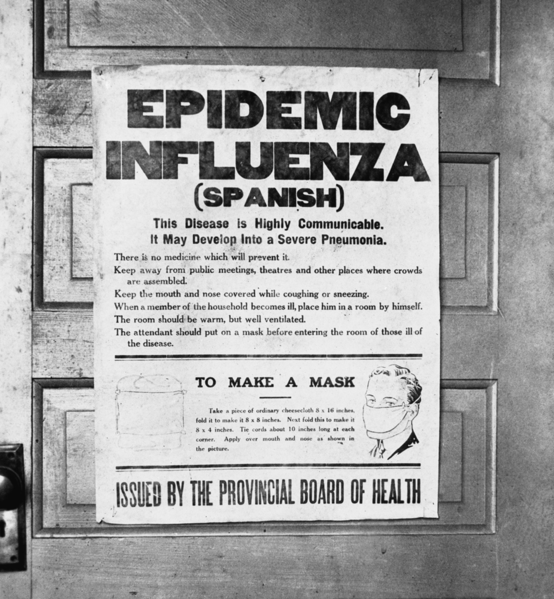
Health alerting the public to the 1918 influenza epidemic. Source:
Alberta Board of Health, Public domain, via Wikimedia Commons
Outside of the lack of a public health care infrastructure, one of the biggest issues when it came to treating influenza patients in Canada was a shortage of health workers. This shortage, however, was not caused by the virus and predated the epidemic. The dearth of health-care workers was due to many trained doctors and nurses serving in the war with the Canadian Corps overseas. For instance, in Vancouver, doctor-to-patient ratios had deteriorated between 1914 and 1918 from 540 patients per doctor to 680. Moreover, the city only had 200 nursing graduates able to work by 1918, and this number quickly dwindled down to 125 by January 1919 as nurses became ill. This experience played out elsewhere too. Initial shortages of doctors in Saskatchewan, due to 74 of 788 local doctors being engaged in military service, were quickly amplified as the remaining doctors became some of the first to get ill treating patients.
The problems the war effort created were not limited to medical worker shortages either. Despite an ongoing epidemic, exceptions were made to public gathering bans in order to conduct drives to sell war bonds. In Vancouver, these drives were held despite the strenuous objections of doctors. In Winnipeg, to support the sale of bonds, soldiers being treated at a military hospital were issued tickets for public events on Oct. 1 and 5. This broke the quarantine imposed on the barracks that was the source of the initial outbreak in the city. This almost certainly escalated the spread within Winnipeg and the city saw infections rise substantially in the later days of October. Even when the war was over, events related to it, such as public celebrations of the armistice in Toronto, have been linked to second waves. Finally, it is important to highlight that factories supplying material for the war effort, such as those in Toronto, continued operating during the epidemic despite the high risk that this would cause further spread. In many ways this last element was particularly important for the ruling class, regardless of the human cost it entailed, because it served two purposes: it ensured the bosses would continue making profits while also supporting the war advancing their interests in Europe.
Social murder and the Epidemic
The way that capitalism amplified the influenza epidemic was not limited to the war. The very conditions that the working class lived in, which arose from the capitalist mode of production, fueled the spread of the virus. It also quite literally led to more deaths. The north of Winnipeg is a tragic example, with that section of the city having a death rate 50 per cent higher than wealthier areas. In Montreal, the city hit hardest by the epidemic, the highest death rate was found in the eastern parts of the city near the river. It is no coincidence that this area had the highest infant mortality rate in Montreal before the epidemic.
Many Indigenous communities across the country were in an even worse position. Already suffering from being forcibly displaced from their traditional lands by British colonialism to make way for the exploitation of natural resources, they also faced several aggravating factors. For one, a number of these communities were still enduring or just recovering from outbreaks of typhoid fever, diphtheria, and other communicable diseases, making them more vulnerable to influenza. Moreover, health-care infrastructure in these communities was often wholly inadequate or completely absent. This issue was only amplified in rural and remote communities such as Norway House near Lake Winnipeg, which had no support in managing outbreaks. It is sadly of little surprise that approximately 18 per cent of the population of Norway House died from influenza in just six weeks.
As all the above shows, the ruling class was aware of these conditions and knew the risk that they would pose. And it was not as if the resources and capability to make improvements were not there. From 1914 to 1918, the Canadian Corps built a complex network of many kilometres of trenches and tunnels under the water-soaked fields of Flanders. This network would play host to more than 100,000 soldiers with sewage systems, water drainage, and field hospitals that could treat hundreds of patients at a time. Yet in many places, with a few exceptions like Toronto, little was done to rectify the problems in the years approaching 1918. These were the conditions that capitalism had created, and they came with a cost that was borne disproportionately by the working class. When Friedrich Engels talked about the idea of social murder in Victorian England in his book The Conditions of the Working Class in England, these are the very conditions he had in mind. When it comes to the many deaths that resulted from the influenza epidemic of 1918, as Engels said, “the offence is more one of omission than of commission. But murder it remains.”
What we can learn from the 1918 influenza epidemic
One of the things that has been continually stressed throughout this article are the commonalities between 1918 and 2020. Just like in 1918, in 2020 medical officials across Canada sent mixed messages about the effectiveness of masks, until coming to a common conclusion on their utility months into the pandemic. Just as in 1918, in 2020 health-care systems were found wanting in many places. This ranged from for-profit care homes cutting corners everywhere, leading to many needless deaths, to hospitals lacking in resources from personal protective equipment (PPE) to beds and ventilators. All this occurred again despite Canadians living in a society that is producing far more commodities and which has made many medical advances in the intervening century. Just like in 1918, in 2020 workers were required to keep on working to make a profit for the bosses, despite this impairing the ability to stop the spread of the virus. This happened in many places, from migrant farm workers in Windsor-Essex continuing to work through outbreaks to industrial bakeries in Toronto that continued operation despite outbreaks being known by public health officials. All these issues are symptoms of another virus: capitalism.

The relevance of the experiences of 1918 to 2020 do not stop there. The decentralized and fragmented health-care system that sought to boot responsibility to other jurisdictions then is the basis for the one that exists now. Yes, it has been built upon, with expansive and more powerful federal and provincial health departments in place. But the issues built into the foundations of the system in 1918 are still there and have reproduced some of the same problems in 2020. It is evident that there is still a lack of coordination in the response to the virus. Moreover, there has been little coordination directing resources to areas of need, leaving provinces and local health units to fend for themselves. This has led to an incoherent situation where some provinces sit on surpluses, while others are experiencing shortages. For instance, some provinces like New Brunswick had testing capacity laying idle and were musing testing old samples in an academic exercise, while Ontario was failing to meet targets. When resources were shifted from province to province, this was done as part of individual acts of political charity, as when Alberta sent PPE to Ontario in April 2020, rather than as part of a coherent plan. This is a health-care system that is not fit for the purpose, and it is one that needs to be torn down and rebuilt to better serve the working class.
One of the most important lessons to take from 1918 is how quickly the bosses forget the lessons of a pandemic and return to their old habits. One great example of this is found in Toronto. Before the pandemic was over, but after the peak of the first wave had subsided, the help the local health department received from the city rapidly diminished and this was soon followed by cuts put forward by the mayor, which included attacks on the health-care infrastructure that had saved lives during the epidemic. In the current pandemic we are seeing the same removal of supports. Rules preventing evictions have been weakened. “Hero” pay for many workers that have been required to continue working on the frontline has been retracted. Wage relief, rent relief, and government grant programs are being put out that serve to line the pockets of the bosses, not the interests of workers.
What we need to do going forward
All this leads to one positive lesson to take from 1918; that workers must be ready to fight to defend their interests. Just as workers were beginning to mobilize in Winnipeg in October 1918 by holding the first general strike vote in the city, workers today must be ready to fight austerity and any attempts to make them pay for the bill for fighting COVID-19. Moreover, it is important to remember that capitalism is the overarching virus of which the current pandemic is just one of many symptoms. When the virus eventually begins to be contained, there cannot be a return to what was business as usual for the bosses. This trajectory that they had us on was one leading us to a climate disaster; one where the living standards of workers everywhere continued to erode while they kept getting richer.
We must throw aside the quackery of reformism for the real cure of socialist revolution. Through this treatment, the working class can build a new health-care system as part of a democratic, planned economy under workers’ control: a health-care system built to serve the interests and the health of the working class. One that would not serve to line the pockets of pharmaceutical company owners. A system that would make sure health-care resources are directed where they are needed most. One that would make sure workers do not have to risk their lives on the front line of a pandemic to pay rent. One that would end the social conditions that allow a virus to spread like wildfire across the world. One that could make this pandemic the last.